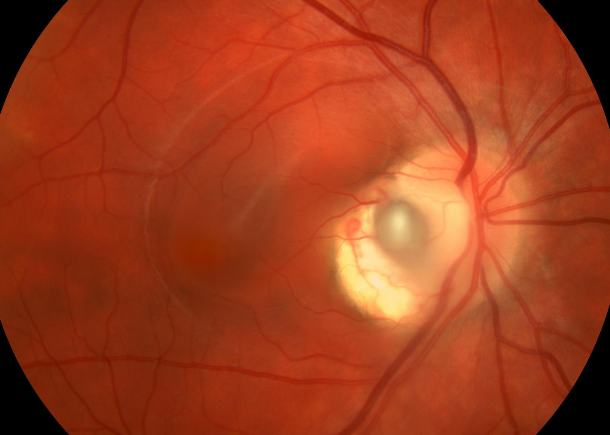
optic nerve pit. The pit is a small defect in the optic nerve that can allow liquid vitreous to enter under the retina, thus potentially causing a retinal detachment and subsequent blindness without proper treatment.
Olivia and her parents, Beth and Andy, started their journey with evaluations from Drs. Thomas France and Yasmin Bradfield, pediatric ophthalmologists in the Department of Ophthalmology and Visual Sciences. They confirmed the condition through diagnostic testing and imaging, then discussed warning signs and possible treatment options if a change in vision was noted. Drs. Bradfield and France also took baseline photos of her optic nerves, should Olivia’s condition evolve later in life. To a young girl who loved dolls and playing outside, this was fairly alarming.
Fast forward to Olivia’s freshman year of high school, where while sitting in class the blackboard lines suddenly bulged and became squiggly. “I waited a full day to tell my parents because I knew what was happening, but I didn’t want this to be happening to me, and I was hoping it would just go away,” says Olivia.
In many cases, patients do not have symptoms for decades. When vision defects do occur, they are caused by an accumulation of fluid within or under the central part of the retina (the macula). No preventative measures can be taken to avoid this fluid accumulation, and treatment can only begin after fluid is present. Even with appropriate treatment, vision may not return to normal.
Because of the information that Olivia and her parents were given six years prior, they could thoughtfully weigh treatment options with Dr. Michael Altaweel, a retinal surgeon. Monitoring was enacted initially for a brief period. Ultimately, the family opted for vitrectomy surgery to stop sub-retinal fluid leakage that had caused a retinal detachment.
Olivia was a novice to surgery, and was pleased with the pain-free outpatient procedure. The recovery, however, was a different story. She had to lay head down for ten days so that the expanding gas bubble injected into her eye would assist in pushing her retina back into place. Her vision was restored to 20/20 – another rarity of this condition and treatment.
“I could not be happier with the results of Olivia’s vitrectomy. The complicated surgery and recovery do not guarantee restored vision,” says Dr. Altaweel. “I am proud to be a part of this team of doctors that communicate throughout a patient’s vision journey to ensure the very best outcomes.”