Two vision researchers at the University of Wisconsin-Madison are involved in groundbreaking research aimed at curing blindness through human eye transplantation.
To date, there has never been a successful whole human eye transplant for the restoration of vision. However, research teams across the country, including at the University of Wisconsin—Madison, are hopeful these efforts will pave the way for this procedure.
Earlier this month, the Advanced Research Projects Agency for Health (ARPA-H), an agency within the U.S. Department of Health and Human Services, announced $125 million in funding from its Transplantation of Human Eye Allografts program. UW researchers are part of two teams that received those contracts.
The two UW researchers involved in the cross-institutional work are David Gamm, MD, PhD and Robert Nickells, PhD. Dr. Gamm is part of the national team led by researchers at the University of Colorado Anschutz Medical Campus that will focus on developing novel stem cell, gene therapy, and bioelectronic technologies to promote nerve regeneration, and also on refining surgical methods. Dr. Nickells is a member of the team from Stanford University. Their focus is on developing new strategies to promote survival and regeneration of cells of the transplanted eye, donor eye procurement, and performing transplant surgeries.
The Challenge
Transplants are not new in the field of ophthalmology. Over 70,000 people in the United States donate their eyes after death each year. However, only parts of the eye, most commonly the cornea at the front of the eye, are used for transplantation. This means that the millions of people blinded by conditions affecting their retina and optic nerve have no options for improvement.
This new initiative aims to address this issue by transplanting the whole donor eye and reconnecting the nerves, muscles, and blood vessels, including the optic nerve, which connects the eye to the brain. If successful, the program will generate new treatments for many leading causes of total blindness in the United States, for which there are currently no cures.
This groundbreaking project aims to achieve the goal of a successful whole eye transplant within six years.
The Gamm Lab
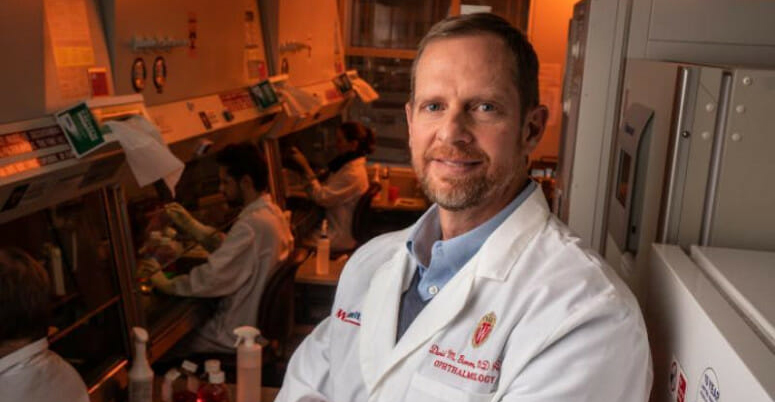
Dr. Gamm and his team of researchers at UW—Madison will explore how to use stem cells to repair and reconnect the optic nerve so the donor eye can communicate with the recipient’s brain and enable vision.
Dr. Gamm, a professor a professor of Ophthalmology and Visual Sciences in the School of Medicine and Public Health and director of the McPherson Eye Research Institute, has been involved in this type of stem cell research for nearly two decades.
His lab has already successfully developed methods to grow authentic retinal cells and tissues from pluripotent stem cells, a powerful type of stem cell that can be used to create any type of cell or tissue in the body.
“To date my lab has primarily been focused on creating ‘spare parts’ of the outer retina – namely photoreceptors and retinal pigment epithelium cells. What is different about this project is the focus on the optic nerve, which is comprised of the axons of retinal ganglion cells. We are trying to create a neuronal connector, consisting of pluripotent stem cell-derived neurons, that can hopefully act as a coupler, to allow communication between the donor eye optic nerve and visual centers of the brain.”
“What we are striving for is a huge undertaking,” Dr. Gamm added. “But, by leveraging the combined expertise of our partners, we expect to make important advances over the next six years.”
The Nickells Lab
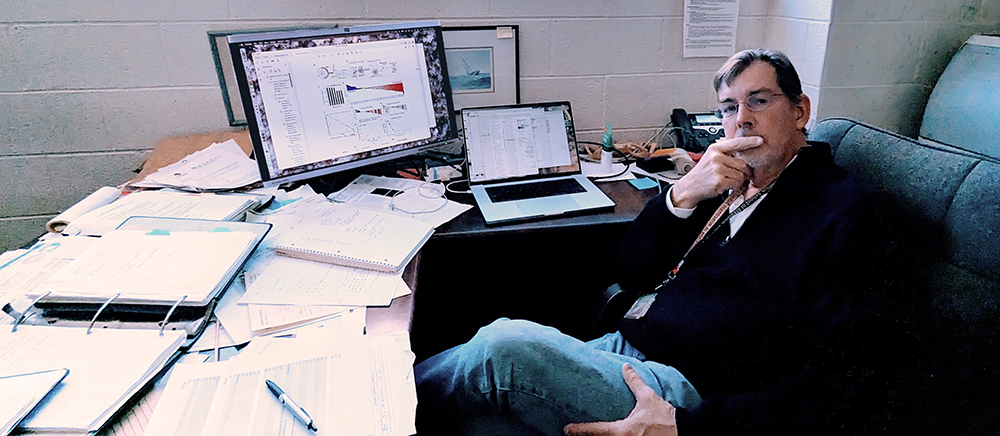
Dr. Robert Nickells, also a professor of Ophthalmology and Visual Sciences in the School of Medicine and Public Health, has been studying whole eye transplantation for more than a decade. His team is developing a cold storage solution that keeps the donor eye healthy between recovery and transplantation. They are specifically focused on maintaining the viability of the donor eye and ensuring the health of the retina, the light-sensitive layer at the back of the eye that sends signals to the brain.
“Our goal is to develop a method of preserving donor retinal tissue for up to 24 hours,” Dr. Nickells said. “Over the last several decades, we’ve been studying the biology of what goes on in retinal cells once they become damaged in the hopes of developing treatments to slow down or block this process. When it came to coming up with a cold storage solution, our first thought was to start with what is normally used in the transplant industry for other organs.”
Surprisingly, the team discovered that UW cold storage solution, developed right here at the University of Wisconsin in the 1970s, was that industry standard.
“While UW solution did fairly well at preserving retinas in our initial studies, we reasoned that we could improve its efficacy by modifying it with supplements that specifically targeted the biochemical pathways that would normally be activated in retinal cells once the donor eye was procured,” explains Dr. Nickells. After testing each supplement individually, the research team came up with a combination that seems to perfectly preserve isolated eyes after prolonged periods in cold storage.
The next step, thanks to the new ARPA-H grant funding, is to examine what happens to the eye, and specifically the highly sensitive retina, once it comes out of cold storage and is warmed up.
“We have some early indications that retinal cells start to regain their function after warming, which is good,” Dr. Nickells continued. “But we also have some indications that the warming process induces a stress response, which may hamper long term survival of the retina after transplantation. Future work may include the addition of further supplements to suppress this stress response.”
“I am honored to be part of this groundbreaking new effort aimed at finding a cure for blindness,” Dr. Nickells added. “The next few years are going to be an exciting time for the field of ophthalmology.”