Vision scientists at the University of Wisconsin—Madison are pioneering a revolutionary approach to eye care by adapting a cutting-edge optical imaging technique from astronomy for use in eye imaging and diagnosis.
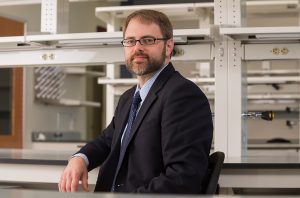
Jeremy Rogers, PhD, along with his team at the Wisconsin Advanced Imaging of Visual Systems (WAIVS) Lab, have harnessed the power of adaptive optics (AO) to dramatically enhance retinal imaging. This breakthrough technology promises to transform clinical practice by providing unprecedented clarity and detail on the cellular level, enabling earlier detection and monitoring of eye disease onset and progression. With this innovative work, Dr. Rogers and his team aim to create a valuable clinical tool that will significantly improve patient outcomes.
Founded in 2018, the WAIVS Lab brings together scientists from the Department of Ophthalmology and Visual Sciences (DOVS), the McPherson Eye Research Institute, and collaborators from the University of Wisconsin and beyond. Dr. Rogers, a scientist with DOVS, is the director of WAIVS and principal investigator of the AO project at UW-Madison.
AO technology was originally developed by astronomers to enhance the quality of telescope images of distant galaxies. In recent years, vision scientists have adapted the technology to capture high-resolution images of retinal cells at the back of the eye. Even with high resolution cameras, imaging these cells is nearly impossible with standard clinical instruments. To address this, Dr. Rogers and the WAIVS scientists use state-of-the-art Adaptive Optics Scanning Laser Ophthalmoscope (AOSLO) technology to turn the eye into a living microscope.
“Adaptive optics technology enables us to see cellular life in the eye that was previously hidden or distorted by natural irregularities,” explained Dr. Rogers. “It enables us to get very detailed information about the individual cells and microscopic structures in the retina, such as photoreceptors, blood vessels, and support structures.”
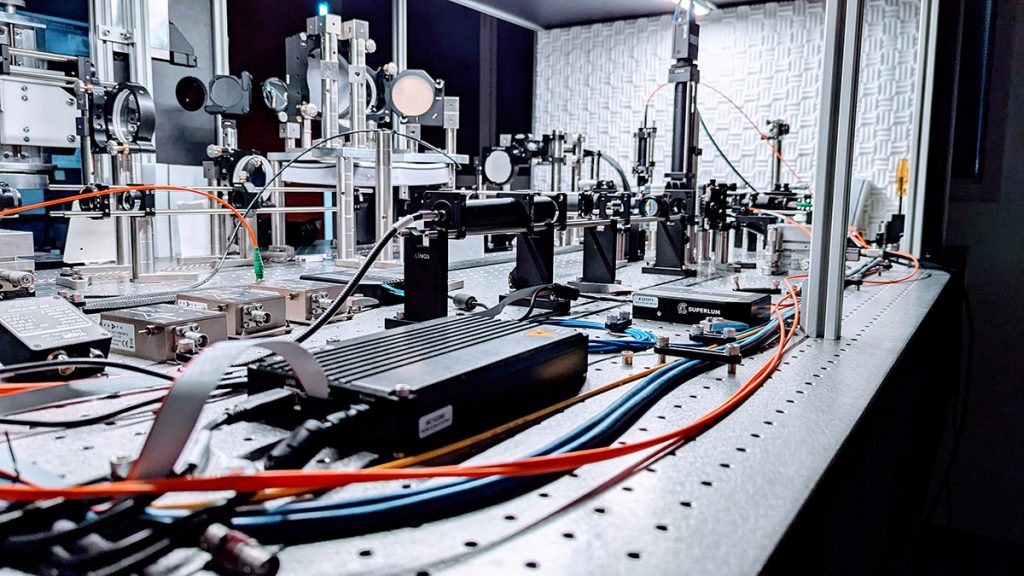
The machines developed at UW-Madison include enhanced capabilities for improved contrast and visualization of retinal photoreceptor cells. The WAIVS Lab houses two such machines.
“The first one is designed for patient research,” Dr. Rogers said. “It allows researchers and clinicians to understand retinal dysfunction on a cellular level in living patients, and also to monitor cellular responses to new future treatments such as stem cell and gene therapies.”
A second machine located nearby, is dedicated to developing and testing innovative features that will allow scientists to “see even further.”
Having the two machines in proximity will allow for rapid application of imaging breakthroughs.
WAIVS is one of only about two dozen institutions in the world undertaking AOSLO research. But the UW-Madison lab is focusing on clinical applicability.
“Many of the instruments used today are optimized to image healthy, young eyes,” Dr. Rogers said. “But the most clinical impact will come from instruments capable of imaging older eyes, or eyes that have undergone surgery, for example.”
Dr. Rogers is developing a compact system that improves the patient experience in several key ways.
“For starters, we want to develop a system that works much faster, reducing the procedure time from 35-60 minutes, to about 5 to 10 minutes,” Dr. Rogers said. “In addition, current systems are somewhat cumbersome. It takes two people to run the instrument, then up to two weeks to process the data. What comes back is not always easy for clinicians to interpret. We want to fix all of that.”
In the end, Dr. Rogers hopes for a system that will lead to earlier disease detection and treatment.
“When we have achieved what we set out to do, we will have accomplished something amazing,” Dr. Rogers said. “It will be a real game-changer.”